The exact pathology of ALS remains elusive to researchers worldwide. However, several genetic factors have been identified as likely components of ALS development. ALS is divided into two types: Familial, and sporadic. Sporadic ALS accounts for roughly 90% of all cases while familial ALS only accounts for 10%. Familial ALS (FALS) is classified as ALS cases in which two or more people in the same family have the disease, Sporadic ALS (SALS) cases are classified as those where only one family member has the disease, and genetic basis for the disease isn’t readily apparent. Due to the fact that FALS more readily lends itself to genetic characterization, it is the more studied of the two types. About half of all familial cases arise from mutations in two genes: the C9orf72 gene, and the SOD1 gene. Roughly 30% of familial cases arise from C9orf72 mutants, and 20% arise from mutations in SOD1. Unfortunately, the effects of the C9orf72 mutations are unclear. SOD1 mutants, on the other hand, have been extensively characterized and remain a central component of ALS research.
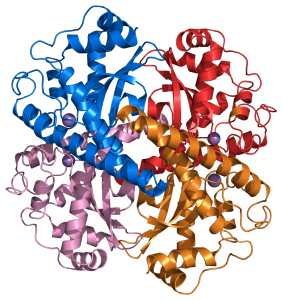
The SOD1 gene codes for a protein called superoxide dismutase (SOD1), which is responsible for reducing a toxic oxidizing agent called the superoxide anion (O-2) into hydrogen peroxide (H2O2), which is eventually reduced to water and oxygen. Research has shown that mutant SOD1 proteins lead to pathological changes in motor neurons associated with ALS, namely excitotoxicity, disturbed calcium homeostasis, oxidative stress, and signals for apoptosis. Excitotoxicity is, perhaps, the best-characterized pathway in ALS pathogenesis with respect to the SOD1 mutation. Excitotoxicity refers to the toxic effect that excessive, prolonged stimulation can have on a neuron. The neurotransmitter (signaling molecule that travels between neurons via the synapse) implicated in ALS pathogenesis is glutamate. Current evidence suggests that excitotoxicity arises due to upregulated Na+ channel activity, which leads to increased release of glutamate by the presynaptic neuron (the neuron transmitting the signal through its axon) into the synapse. This, in turn, leads to increased calcium concentration in the postsynaptic neuron (the neuron receiving the signal through its dendrites), which alters mitochondrial function in that neuron. The overstimulation eventually leads to dysfunction and death of the neuron, but the exact link with SOD1 is still unclear.
Part of what makes pathogenic identification so difficult is the fact that we don’t exactly know the etiology of the disease. In fact, the etiology may be different for many types of ALS, and they all just happen to result in the same neurological deficit in motor neurons. In FALS it is currently believed that mutated genes start the cellular machinery of the primary disease process early in life and that individuals are asymptomatic until their compensatory mechanisms are overwhelmed by trauma or environmental factors.

(Figures 2 & 3). Steve Gleason, a former NFL star, was diagnosed with ALS at age 34. It is believed that he had a genetic predisposition towards the disease, but that repeated concussions may have been the ultimate trigger.
The pathogenesis of SALS is more difficult to characterize. However, it is encouraging to note that many of the wild-type counterparts of mutant proteins (particularly SOD1) from FALS are implicated in SALS as well. In particular, researchers have found that the mRNA coding for wild-type proteins are present at significantly higher levels in the brainstem and spinal cord in SALS patients than in unaffected individuals. The significance of this is twofold: First, this means that environmental factors may upregulate SOD1 protein production even when the genes aren’t mutated, which may result in neurological damage. Second, it shows that ALS may be more closely linked to the mutations causing increased production of the protein rather than those that cause a protein with an altered amino acid sequence.
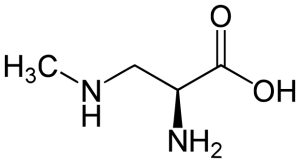
The fact that ALS currently appears to have an etiology involving more than genetic factors has kept researchers on the hunt for environmental triggers, which is why algal blooms have become a topic of interest in North America. Cyanobacteria in freshwater lakes produce a compound called BMAA (beta-Methylamino-L-alaine), which is a suspected environmental trigger involved in the onset of ALS. In vitro, BMAA has been shown to have an excitotoxic effect on glutamate receptors, which would lead to neuron dysfunction through the pathway mentioned above. In addition to algal blooms, BMAA is also found in cycad seeds. More specifically, cyanobacteria live in the roots of these plants, and BMAA from the cyanobacteria can be incorporated as chemical components of the seeds. People can obtain significant levels of BMAA in their bodies through direct ingestion of the cycad seeds, but secondary ingestion is, perhaps, an even more significant exposure route. It turns out that appreciable levels of BMAA have been found in the flesh of animals that have consumed the seeds, so subsequent consumption of these animals can result in exposure to BMAA as well. An ALS cluster on the island of Guam is believed to have arisen, at least partially, due to primary or secondary ingestion of BMAA from cycads. Flying fox bats from Guam, which include cycad seeds in their diet, were found to have significant levels of BMAA in their systems. They also happen to be a delicacy on the island, which opens up an exposure pathway. It is important to note that BMAA cannot be destroyed by cooking.
Figures were found at the following links:
Figure 1: https://en.wikipedia.org/wiki/Superoxide_dismutase
Figure 2: http://www.athletepromotions.com/blog/former-new-orleans-saints-player-steve-gleason-speaks-about-als/17422/
Figure 3: http://www.espnfrontrow.com/2013/10/pearl-jam-provides-soundtrack-to-life-of-former-nfler-steve-gleason/
Figure 4: https://en.wikipedia.org/wiki/Beta-Methylamino-L-alanine#/media/File:3-Methylamino-L-alanine.svg
References:
- Beghi E, Mennini T; Italian Network for the Study of Motor Neuron Disease. 2004. “Basic and clinical research on amyotrophic lateral sclerosis and other motor neuron disorders in Italy: recent findings and achievements from a network of laboratories”. Neurol Sci 25 Suppl 2:S41-60.
- Gagliardi S, Emanuela C, Davin A, Guareschi S, Abel K, Alvisi E, Laforenza U, Ghidoni R, Cashman JR, Ceroni M, Cereda C. 2010. “SOD1 mRNA expression in sporadic amyotrophic lateral sclerosis”. Neurobiology of Disease 39(2):198-203.
- Manfredi G, Zuoshang X, 2005. “Mitochondrial dysfunction and its role in motor neuron degeneration in ALS”. Mitochondrion 2005(5):77-78.
- Mühling T, Duda J, Weishaupt JH, Ludolph AC, Liss B. 2014. “Elevated mRNA-levels of distinct mitochondrial and plasma membrane Ca2+ transporters in individual hypoglossal motor neurons of endstage SOD1 transgenic mice”. Frontiers in Cellular Neuroscience 353(8):1-14.
- Van Zundert B, Izaurieta P, Fritz E, Alvarez FJ. 2012. “Early pathogenesis in the adult-onset neurodegenerative disease amyotrophic lateral sclerosis”. J Cell Biochem 113(11):3301-12.
- Carriedo SG, Yin HZ, Weiss JH. 1996. “Motor neurons are selectively vulnerable to AMPA/kainate receptor-mediated injury in vitro”. J Neurosci 16(13):4069-79.
- Banack SA, Murch SJ, Cox PA. 2006. “Neurotoxic flying foxes as dietary items for the Chamorro people, Marianas Islands”. J Ethnopharmacol 106(1):97-104.
- Cox PA, Sacks OW. 2002. “Cycad neurotoxins, consumption of flying foxes, and ALS-PDC disease in Guam”. Neurology 58(6):956-9
- Arens NC. 1995. “Cycads: Life History and Ecology”. UC Berkeley. website url: <http://www.ucmp.berkeley.edu/seedplants/cycadophyta/cycadlh.html>